A healthcare team at Oregon Health & Science University is experimenting with a novel approach to treating patients who have hepatitis C or are at risk of developing it. The goal is to help patients overcome obstacles that would otherwise make it seem impossible to receive testing and treatment.
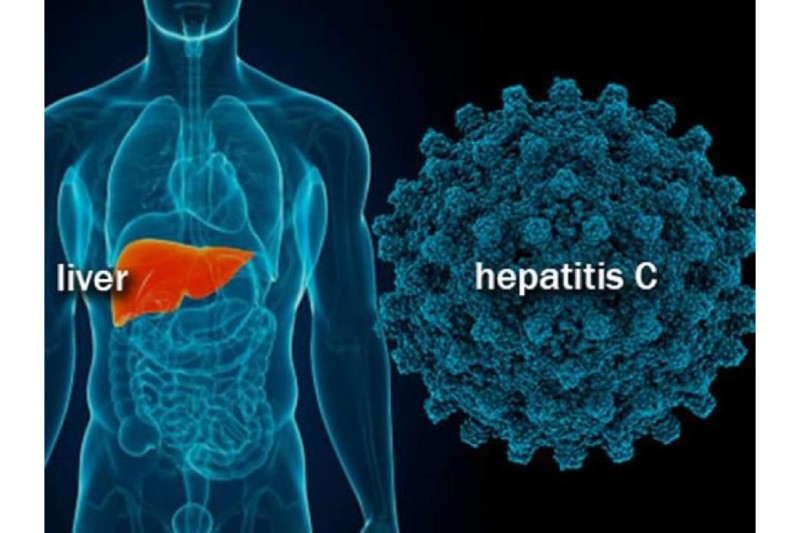
The team is halfway through a one-year pilot project that helps already-hospitalized patients get tested for and treated for hepatitis C-related liver injury—a condition that can be cured with consistent treatment but does not have a vaccine. OHSU’s pilot, called hepatitis C Transition-to-Treatment, looks to end the cycle of delayed care for some of its weak patients, who battle with substance use disorder, unstable housing and other challenges.
“A number of patients have become tearful when we’re discussing treatment,” said Jane Babiarz, M.D., an associate professor of medicine (general internal medicine and geriatrics) in the OHSU School of Medicine and one of the pilot project’s organizers. “Patients have said, ‘I never thought I was going to get treated for hepatitis C. No one has ever treated me like a person before or acted like this matters.'”
Six of the 19 patients who participated in the pilot have completed their treatment within the first seven months. The clinical team anticipates that participants who have completed treatment will soon be tested for hepatitis C.
Prioritizing hep C treatment
An expected 2.4 million individuals in the US have hepatitis C, and the greater part don’t realize they have it. The condition is more common in individuals who use injectable drugs since it’s often spread by sharing needles. Treatment is an essential component of preventing transmission because there is no hepatitis C vaccine. People can get rid of the hepatitis C virus with antiviral medications, but they usually need to be taken every day for two to three months.
Patients who are also struggling with a substance use disorder may find it especially difficult to adhere to a treatment program. are experiencing homelessness or unstable housing; have limited access to transportation; or face other stigmatizing issues. Despite the fact that patients with hepatitis C are more likely to be admitted to the hospital for a variety of other health issues, medical professionals typically concentrate on treating the patients’ more urgent needs and postpone providing treatment for hepatitis C until a later time.
For the overwhelming majority weak patients, that can mean postponements of years, on the off chance that not many years. In the event that hepatitis C isn’t dealt with, it tends to be spread to other people, and can prompt liver cancer, cirrhosis or end-stage liver disease years later.
By providing treatment to patients who are being admitted to OHSU Hospital for another health issue, the pilot program at OHSU aims to break the cycle of delayed care. The project specifically aims to assist unhoused, drug-using, or mentally ill hospitalized patients who may be unable to receive treatment. Carissa Williams, LCSW, M.P.H., an OHSU Clinical Outreach Social Worker, visits the hospital room of a patient who has tested positive for hepatitis C to talk about the program and determine whether or not the patient is ready for treatment.
Patients who enlist then, at that point, have virtual encounters with Babiarz through video or calls from their hospital rooms. Babiarz partners with infectious disease pharmacists HaYoung Ryu, Pharm. D., YoungYoon Ham, and Pharm.D., to recognize expected patients for treatment and speed up approval.
The majority of people who are given antivirals start treatment while they are still in the hospital. After patients are released, Babiarz and Williams keep on meeting with them and guarantee they have the help they need. In addition, Williams meets with patients in the community to offer support, link them to resources, and address obstacles to finishing treatment. 90 days subsequent to finishing treatment, a subsequent blood test is led to affirm the virus is gone.
“This is a real opportunity for ingenuity in medicine,” Babiarz said. “We’re using a human-focused approach to eradicate hepatitis C, without making vulnerable patients jump through unnecessary, ineffective hoops.”
OHSU research identifies a need
The pilot’s strategy is supported by OHSU research. All adults should be tested for hepatitis C at least once in their lifetime, and those with substance use disorders should have their tests performed more frequently.
Notwithstanding, an OHSU-led study recently published in Therapeutic Advances in Infectious Disease tracked down testing for this and different infections, like syphilis or Human Immunodeficiency Virus, or HIV, changes in patients who have substance use disorder and are hospitalized for bacterial infections. Just 80% of studied patients who didn’t have an earlier hepatitis C diagnosis were evaluated for the virus.
The study found that only about 24% of the patients it tracked had a primary care provider, despite the fact that primary care clinics are intended to assist patients in preventing and managing chronic health conditions.
“Many who experience unstable housing or have substance use disorder have had negative health care experiences, and may not trust health systems enough to become a patient at a primary care clinic,” said Cara Varley, M.D., M.P.H., an assistant professor of medicine (infectious diseases) in the OHSU School of Medicine and the OHSU-PSU School of Public Health, and a lead author of the study.
“As a result, many only seek care when something is urgent enough that they need to go to an emergency room. Hospitalization offers a unique opportunity to address potentially life-threating conditions like hepatitis C and also help decrease the spread of infectious diseases in our community.”
Patients’ experiences were documented in a previous qualitative study conducted by Ximena Levander, M.D., M.C.R., assistant professor of medicine (general internal medicine and geriatrics) at the OHSU School of Medicine. Varley’s findings support those experiences. That’s what the review inferred, with shifting requirements among individuals who use drugs, hospitalization is a vital chance to address hepatitis C considerations, including treatment qualification, solidification of care and help of references. The pilot’s mediation configuration depends on these discoveries.
The pilot project started enrolling participants in July 2022 and expects to select, and ideally fix, 25 patients through June 2023. It’s right now supported by a grant from OHSU Health Integrated Delivery System, a network that spotlights on meeting the necessities of OHSU patients who are covered by Medicaid. Babiarz and his colleagues hope to continue their work after the summer is over by presenting their findings to leaders at OHSU and nonprofit organizations.

 Neurology2 weeks ago
Neurology2 weeks ago
 Cardiology2 weeks ago
Cardiology2 weeks ago
 Cardiology2 weeks ago
Cardiology2 weeks ago
 Cardiology2 weeks ago
Cardiology2 weeks ago
 Neurology2 weeks ago
Neurology2 weeks ago
 Neurology2 weeks ago
Neurology2 weeks ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Neurology1 week ago
Neurology1 week ago