There is evidence of a connection between the two illnesses, according to an American study. Iron affects the microbiota, immune system, and risk of illness.
About 1% of people have celiac disease, a chronic autoimmune condition that usually develops in genetically susceptible individuals. There are 245 thousand certified instances of celiac disease in Italy, but there may be as many as 600 thousand cases among the “underground” (undiagnosed) population. Approximately 9,000 new cases are diagnosed each year.
Low Levels of Iron
A study conducted in the United States and published in BMJ Open Gastroenterology has demonstrated and validated a connection between iron deficiency and celiac disease. Based on a review of 336 thousand individuals, 1,855 of whom had celiac disease, the authors from Harvard Medical School in Boston and the University of Washington in Seattle found that a genetically lower iron level is linked to an increased risk of celiac disease. disease.
Environmental and Genetic Variables
Owing in part to more accurate diagnosis, the prevalence of celiac disease has grown in recent years. The DQ2 and DQ8 haplotypes are hereditary, but the environmental factors also function as triggers. Some studies list the duration of nursing, gluten exposure, prenatal variables, illnesses (including rotavirus), socioeconomic factors, geographic location, microbiome composition, and medications among the latter. None of these elements, however, have offered indisputable proof or helped to avoid celiac disease.
Both Celiac Disease and Anemia
Conversely, low iron levels are preventable; they are the most prevalent nutritional deficiency worldwide, impacting both high- and low-income nations. The authors of the new study claim that the rise in celiac disease diagnoses in the US has coincided with an increase in iron deficiency, which is also caused by a lower intake of the mineral in the diet. Additionally, anemia is more common in the populations most impacted by the condition, including children, adolescents, and women who are not yet menopausal.
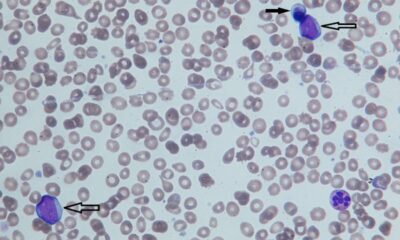
Intricate Connection
Up to 80% of patients of celiac disease also have iron deficiency, and there is mounting evidence that the two disorders are intricately related. The main cause of iron insufficiency in celiac disease has frequently been linked to impaired iron absorption brought on by duodenal mucosal atrophy. Nevertheless, the duodenum can only absorb 10% of the iron in food to meet the body’s requirements. Consequently, it is unlikely that a decreased mucosal surface area is the primary reason for the insufficiency, unless the diet is exceptionally inadequate.
The Receptor for Transferrin
Another protein that is involved is called transferrin receptor 1, and its level rises when an iron deficit occurs. According to one study, individuals with both iron insufficiency and celiac disease had far greater receptor levels than those who only had iron deficit.
Defense Mechanism
Iron’s effects on the innate immune system, infection risk, and microbiome are hypothesized to play a role in the onset of celiac disease. Two iron-metabolizing proteins, hepcidin and lactoferrin, are implicated in innate immunity. Iron deficiency has been demonstrated to affect the microbiome, which in turn affects the onset of celiac disease. Recent research has demonstrated the vital function iron plays in controlling the immune system in the intestine, suggesting that iron deficiency may contribute to inflammatory bowel illnesses and other immune system problems.

 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology7 days ago
Diabetology7 days ago
 Diabetology17 hours ago
Diabetology17 hours ago