Hypoxia, or a shortage of oxygen, is terrible news for the majority of our tissues and cells. However, in these hypoxic conditions, cancer cells can proliferate, making tumours less responsive to anti-cancer therapies like radiation. The defences that cancer develops as a result of hypoxia may now be overcome according to recent studies.
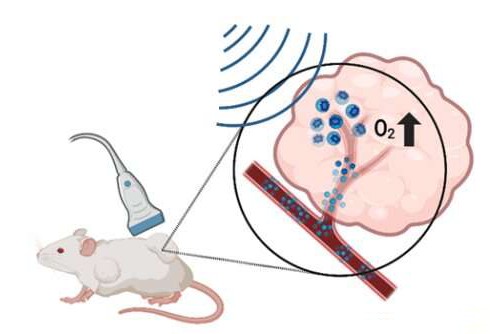
Researchers at Thomas Jefferson University and Drexel University have developed a method to deliver oxygen and cancer treatments to tumours using ultrasound and microbubbles. Their study’s findings, which were reported in Pharmaceutics, show that the approach, which was tried out on mice, primed tumours to be more susceptible to radiation therapy, which slowed tumour growth and improved survival. The study authors recommend that with additional development, their methodology could be used to improve the viability of radiation treatment in the clinic for various cancers.
“At the moment there’s very little we can do on the clinical side to overcome hypoxia for radiation therapy, despite it being a well-known and documented limitation,” said study author John Eisenbrey, Ph.D., an associate professor of radiology at Thomas Jefferson University. “The hope is that a more localized, more aggressive targeting of hypoxia, like what we’ve done here, will overcome some of that.”
More than half of all cancer patients are treated with radiation therapy, which is also known as radiotherapy. This treatment has been a staple of cancer management for a long time. High doses of radiation are used by doctors in this method to kill cancer cells.
Eisenbrey stated that hypoxia is one of the primary reasons why many tumors resist radiotherapy.
“Whenever I say we’re delivering oxygen to tumors, a lot of people say, ‘Well, that’s crazy. You’re going to encourage them to grow,'” said study co-author Margaret Wheatley, Ph.D., a professor of biomedical engineering at Drexel University. But radiation therapy, which prevents cancer cells from replicating, requires an ample supply of oxygen close by to be effective, she explained.
Wheatley, Eisenbrey, and their colleagues devised a strategy to overcome radiotherapy resistance that makes use of tiny, delicate bubbles, or microbubbles, about the size of red blood cells, to make tumors more responsive to radiotherapy.
They packed oxygen molecules into the microbubbles to raise oxygen levels in tumors. They also added the drug lonidamine, which stops cancer cells from using oxygen for their own benefit, to stop cancer cells from doing so.
The microbubbles are injected and circulated throughout the body after assembly, releasing only their intended payload at healthy tissues. The secret to the designated discharge is ultrasound. The researchers are able to pop and release the contents of the microbubbles that have traveled to a tumor by directing ultrasound waves specifically at it.
The method was used to treat breast cancer-derived tumors in mice in a previous study, and the results were encouraging. In the new work, they went above and beyond by focusing on head and neck cancer cell-derived tumors.
“They are notoriously more hypoxic than other solid tumors and also relatively resistant to radiation therapy,” Eisenbrey said.
The researchers gave mice metformin, a drug known to slow cancer growth, orally, injected them with oxygen and lonidamine-filled microbubbles, and then used ultrasound to burst them at the tumor site. Different groups of mice were given not exactly the full treatment, not getting one or a significant number of the elements of the system preceding radiotherapy.
The researchers monitored the tumors’ size over the next three months after exposing the animals to radiation.
Tumor growth slowed to varying degrees in each group that received some form of treatment. Prior to radiotherapy, the mice treated with fully loaded bubbles and metformin lived the longest and saw a significant halt in tumor growth. The increase in oxygen within the tumors made them more susceptible to radiation treatment, according to the authors.
Even in mice, progress against head and neck cancer is very encouraging, according to Eisenbrey. However, the team intends to continue fine-tuning the approach by streamlining the production of microbubbles and optimizing drug and radiation doses for improved outcomes, bringing their cancer patients’ solution closer to reality.
“The authors are using ultrasound and microbubbles in an innovative way, delivering oxygen and drugs to tackle a very serious clinical dilemma. They obtained some promising results, so I’m curious to see how this approach fares with additional development,” said Randy King, Ph.D., director of the ultrasound program in the Division of Applied Science and Technology at the National Institute of Biomedical Imaging and Bioengineering (NIBIB).

 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology2 weeks ago
Diabetology2 weeks ago
 Diabetology1 week ago
Diabetology1 week ago
 Diabetology2 weeks ago
Diabetology2 weeks ago